Cervical spinal stenosis is basically the narrowing of the space available for the spinal cord and/or nerve roots in the neck.
The spinal cord is analogous to the “highway nerves”, and the nerve roots are analogous to “exit road nerves”. The spinal cord or highway nerves control a much larger area of the body, whereas the nerve roots or exit road nerves control specific areas of the arms.
If cervical spinal stenosis causes spinal cord compression, it is known as cervical myelopathy. If cervical spinal stenosis causes nerve root compression, it is known as cervical radiculopathy.
Contributing Factors

Figure 1
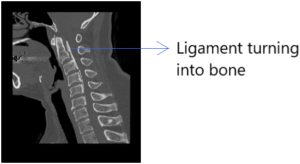
Figure 2
Common Symptoms
Diagnosis
X-rays – reveal structural changes, such as loss of disc height, bone spurs, presence of ossified posterior longitudinal ligament, and mal-alignment (signify abnormal motion and perhaps instability) of the spine.
MRI – allows a closer assessment of any evidence of compression of spinal cord and nerves, and if there are, what are the offending structures (e.g. discs, bone spurs, thickened ligaments).
Nerve and Muscle Electrical Studies – Nerve conduction test assesses the peripheral nerves in the upper and lower limbs. It measures how electrical impulses are conducting in the nerves. These electrical impulses conduction will be affected and slowed if the nerve is diseased, damaged, injured or compressed. Whereas, muscle electrical study is a test which is conducted to study the electrical activity of muscle fibers individually and collectively via needle electrodes.
Treatment
Non-Surgical
Most people with cervical spinal stenosis which involve only the nerve roots (cervical radiculopathy) do not need surgery.
Nonsurgical treatment can be started first, and they are fairly effective in reducing pain and other symptoms. Examples of non-surgical treatment include the use of various types of medications, including non-steroidal anti-inflammatory medications and nerve stabilizers. Treatment may also include passive and active physical therapies and perhaps acupuncture.
Spinal Injection
The doctor may recommend spinal injections if the above-mentioned treatment does not adequately relieve the symptoms.
The spinal injections are performed as a day procedure under the CT guided scan to ensure accuracy and safety when doing the spinal injections. The injections will target the structures which are responsible for the symptoms (for example, the nerve roots, facet joints, and the discs). The nerve roots and facet joints can be injected with a mixture of long acting local anesthetics and steroids. Radiofrequency will also be applied to the discs to reduce the protrusion of the discs in selected cases.
Surgery
Surgery may be considered if non-surgical treatments are not effective. It can also be recommended if the symptoms worsen, which may happen swiftly or insidiously over time.
In cases of cervical spinal stenosis which involve the spinal cord (cervical myelopathy), surgery is often the first treatment recommended due to the progressive deteriorating nature of the condition. This is especially so if MRI shows signs of spinal cord damage, for example, spinal cord swelling (Figure 3).
The objective of surgery is to decompress the compressed spinal cord and/or nerves. There are different types of decompression procedures to treat spinal stenosis affecting the spinal cord and/or nerve roots. The Doctor will recommend either the anterior approach or posterior approach.

Figure 3
(i) Anterior Approach
Surgery from the front (anterior approach) is indicated if the levels of spinal cord/nerve root compression do not exceed three levels and the compression is from the front of the spinal cord/nerve roots.
Anterior cervical decompression and fusion involves approaching the cervical spine from the front and removing any discs, bone spurs, or other structures that are compressing the spinal cord and nerve roots. It typically includes fusing one or more levels of the cervical spine to maintain spinal stability. If only the discs are removed, then the procedure is called anterior cervical discectomy and fusion (Figure 4). If the vertebra as well as the discs are removed, then the procedure is called anterior corpectomy and fusion (Figure 5).

Figure 4 - Anterior cervical discectomy and fusion

Figure 5 - Anterior corpectomy and fusion
Sometimes, instead of fusing the front portions of the cervical spine after removing the discs, the doctor may insert artificial disc implants. This is called cervical disc replacement or arthroplasty (Figure 6). Hybrid procedures may also be performed, where one level of the cervical spine is fused and another level replaced with cervical disc replacement or arthroplasty (Figure 7).

Figure 6 - Cervical disc replacement

Figure 7 - Hybrid procedure
(ii) Posterior Approach
Surgery from the back of the neck (posterior approach) is indicated if the levels of spinal cord / nerve root compression exceed three levels.
A cervical laminectomy involves approaching the cervical spine from the back and removing the back portion of the vertebra (bony arch or lamina) in the neck to create more room within the spinal canal. This may be combined with foraminotomies, where the Doctor creates more room for the spinal nerve roots. This procedure is often combined with instrumentation where screws are inserted into the cervical spine to provide more stability (Figure 8).

Figure 8
Sometimes, if the spinal cord compression is very severe, the Doctor may recommend combined posterior and anterior approaches. This is usually done as a staged procedure, i.e. at different timings (Figure 9).

Figure 9
Laminoplasty (non-fusion procedure) can be an alternative to laminectomy. It opens up the space within the spinal canal by creating a hinge on the lamina of the cervical spine. Titanium mini plates and screws bridge the gaps in the opened sections of the cervical spine (Figure 10). This procedure preserves the spinal motion and lessens the stiffness that may occur after laminectomy and fusion. However, this procedure is not suitable if the spine has mal-alignment or instability.
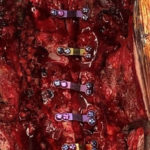
Figure 10(i)

Figure 10(ii)
