With great strides made in cancer management, many patients affected with the once feared disease can expect to live much longer than ever before.
With increased longevity, we are seeing more patients having cancer involving the spine. The skeleton is most commonly affected by cancer. Nearly one-third of skeletal tumours are located in the spine, making the spine the main bony target for tumours.
Possible modes of tumour spread include transmission through the arterial or venous system, through the cerebrospinal fluid of the brain and spinal cord, or via direct extension to neighbouring structures.
The common cancers that will spread to the spine include breast, lung, prostate, thyroid, kidney, gastrointestinal, and bladder.
The disabilities from spinal tumours can be severe. The disabilities are mainly due to spinal collapse (from the weakening of the vertebra due to tumour invasion) and spinal cord / nerve compression from the tumour.
Presenting symptoms will include pain, weakness, gait abnormalities, numbness and bladder disturbances. If the patient has a history of cancer and experiences any of the above symptoms, this constitutes an emergency.
Diagnosis
MRI (Magnetic Resonance Imaging) is the gold standard in imaging of spinal metastasis (Figure 1). It provides accurate information about the involvement of the soft tissue and bony structures by the tumour. It also defines the presence and degree of spinal cord compression and nerve root impingement. Contrast injection may be needed, as it further provides a clearer definition of soft-tissue invasion by the tumour along with how much blood supply the tumour is receiving.
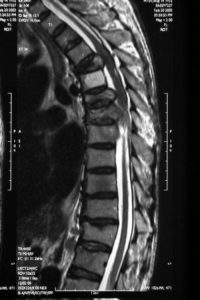
Figure 1
CT scan may be ordered as it is useful in determining spinal stability that may be caused by the tumour spread. CT easily differentiates bone from soft-tissue tumour extension. This finding may play a significant role in determining whether the patient will require surgery or radiation therapy.
Bone scan detects regions of remodelling (process of bone breakdown followed by formation of new bone) in the skeletal system (Figure 2). Although remodelling may be associated with bony tumours, it may also be the result of inflammation, infection, or fractures
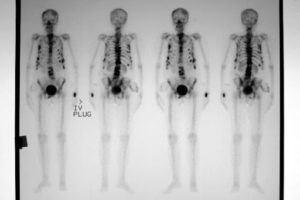
Figure 2
PET scan (Positron Emission Tomography) employs tagged molecules to detect regions of increased uptake. 18Fluorodeoxyglucose (18FDG) is commonly used in PET scan, and it aggregates in regions of increased metabolic activity in the skeleton and soft tissues. PET scans are useful in staging the extent of the systemic disease (Figure 3).
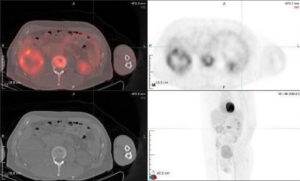
Figure 3
Treatment
Improvements in adjuvant therapy have led to a decrease in surgery for spinal tumour in favour of radiation therapy. However, surgery still continues to play a critical role in the treatment of spinal tumours. The goals of surgery include the preservation or restoration of nerve function and stability of the spine.
Traditional open surgery for spinal tumours involves decompression (freeing up) of the compressed nerves, followed by stabilization with titanium screws and rods. The stabilization may be augmented with cage and/or cement.


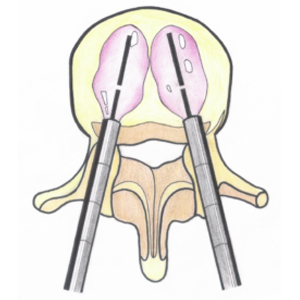
In selected cases, minimally invasive stabilization can be performed in cases of impending or established spinal instability due to tumour destruction of the vertebral body. This can be done via small stab incisions, thereby leading to significant reduction of morbidities. If concurrent decompression is necessary, an additional midline incision can be made to achieve it.
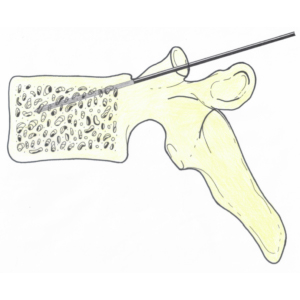
Some of the spinal tumours do not present with impending spinal cord compression or instability, but are painful. In such instances, injection of bone cement under x-ray guidance is a good method to restore spinal instability and reduce the pain and disability (Figure 5).

Figure 5
In spinal tumour cases, the spine doctor will work together with the treating medical and radiation oncologists in the decision making to formulate the best treatment option for the patient.
