Lumbar spinal stenosis (narrowing of the space for the nerve in the lower back) is a condition affecting mainly the middle aged and beyond.
It happens because of gradual narrowing of the space for the nerves. One of the functions of the spinal column in our body is to facilitate passage and exit of various nerves. The nerves in the lower back or lumbar spine mainly travel to the legs, and they serve both motor (giving instructions to the muscles in the legs to move) and sensory (receiving various sensory feedback from the skin of the legs) functions. Some of the nerves that travel in the lower back spinal column are responsible for control of the bladder and bowel.
Contributing Factors

Figure 1

Figure 2
Common Symptoms
Diagnosis
X-rays – reveal structural changes, such as loss of disc height, bone spurs, and mal-alignment (signify abnormal motion and perhaps instability) of the spine.
MRI (Figure 3) – a closer assessment of any evidence of compression of the nerves, and if there are, what are the offending structures (e.g. discs, bone spurs, thickened ligaments).
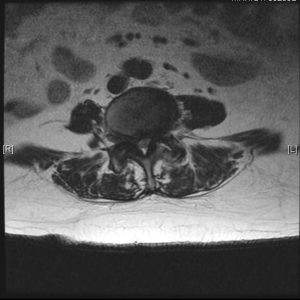
Figure 3
Treatment
Non-Surgical
In the absence of severe or progressive nerve damage, the doctor will usually manage spinal stenosis using the following non-surgical measures:
Spinal Injection
The doctor may recommend spinal injections if the above non surgical treatments do not adequately relieve the symptoms. Spinal injections or nerve root blocks near the affected nerve(s) are done to temporarily relieve pain and nerve inflammation. This can be done as a day surgery procedure in the operating room where sterility is ensured and imaging access to the spine is available. At the same time, injections into the facet joints and the medial branch nerves (nerve supply to the facet joints) may also be done to relieve inflammation of the facet joints.
Surgery
Surgery should be considered immediately if one develops numbness or weakness that interferes with walking, impaired bowel or bladder function. Otherwise, surgery may be considered if there are no significant improvements with non surgical treatments, or the quality of life is significantly affected.
The purpose of the surgery is to relieve pressure on the nerves (decompression), as well as restore and maintain alignment of the spine at times (stabilization). Such procedures can be done via minimally invasive techniques using specially designed tubular systems.

Figure 4
