Teenage or adolescent idiopathic scoliosis (AIS) affects children between ages 10 to 18. The incidence rate is about 3 – 4% in our school children.
The scoliosis usually worsens during the rapid growth period of the patient. While most scoliosis stop progression at the time of skeletal maturity, some, especially curves greater than 50 degrees, continue to progress during adulthood.
“Idiopathic” means that the condition has no identifiable causes although there may be some genetic basis for AIS. Approximately 30% of AIS patients have some family history of scoliosis.
Although idiopathic scoliosis occurs most often in the teenage years, it can also present in younger age groups, i.e. 9 years and younger. These idiopathic scoliosis cases are also classified as early onset scoliosis (EOS). Apart from idiopathic cases, EOS also encompassed other rarer forms of scoliosis, e.g. congenital scoliosis (present at birth due to abnormal development of the vertebra), neuromuscular scoliosis (e.g. spinal muscular atrophy), and syndromic scoliosis (e.g. neurofibromatosis). There is a greater tendency of the scoliosis in EOS cases to worsen, as compared to adolescent idiopathic scoliosis. Special considerations for surgical treatment are required, as the child has many years of growth remaining.
What are the common features of AIS?

Figure 1
When to see a Doctor?
Go to a medically trained spine specialist if you notice signs or symptoms of scoliosis in your child. However, mild curves can develop without the parent and child knowing it because they appear gradually and usually do not cause pain.
Assessments
Treatment Options
Observation
Bracing

Hard Brace
Surgery
Types of Surgery
(A) Fusion
Fusion is the most commonly adopted surgical method of choice, where the vertebrae are joined together by bone implanted during surgery and held together by titanium screws and rods. The surgery can be performed with either from the back or side of the body. For the back approach, a straight incision is made along the midline of the back.

Double Curves (i)

Double Curves (ii)
For the side approach, an incision is made through the side of the spine. This side approach is an option in cases where a single thoracic curve or a single lumbar curve is being surgically treated.

Single Thoracic Curve

Single Lumbar Curve
(B) Non-fusion
(i) Apifix
For some adolescent idiopathic scoliosis, there may be a role for non fusion Apifix surgery if the spinal curvatures are less than 60 degrees, and are also flexible. The surgery involves a dynamic deformity correction system which acts as an internal brace implanted unilaterally on the concave side of the curve. The operating time is significantly shorter than the traditional scoliosis fusion surgery. This translates to shorter hospital stay and shorter downtime to resumption of daily activities of living.
Non-fusion Apifix Surgery
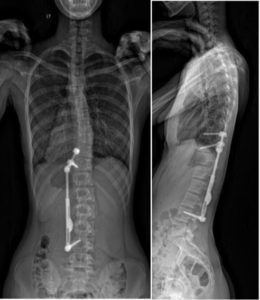
(ii) Growing Rods
Growing rods are used in the surgical treatment of Early Onset Scoliosis patients, and the device can be adjusted in tandem with the growth of the child. A final surgery involving fusion will be performed to correct and stabilize the scoliosis.

Non-fusion Surgery using Growing Rods
What happens if Scoliosis is left untreated?
Moderate to severe scoliosis that is left untreated can lead to pain and increasing deformity, as well as potential heart and lung damage. It may also exert profound psychological impact on the patient due to the physical appearance.
